The Montreal Model
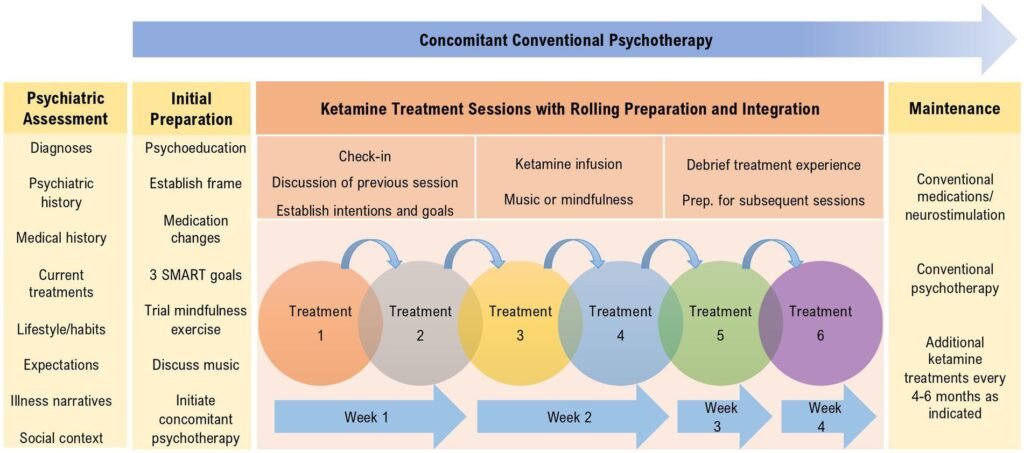
The Montreal Model of Ketamine Therapy is an intensive, evidence-based program that combines low-dose ketamine treatments with psychological support and behavioural changes to help patients recover from treatment-resistant depression (TRD). It aims to use the rapid but often temporary antidepressant effects of ketamine as a window of opportunity that, in synergistic combination with psychotherapy and psychedelic-like treatment settings, can facilitate lasting psychological growth and recovery.
Learn more
The Ketamine Chameleon
Ketamine’s mind-altering effects have long sparked fascination and debate. Is it a dissociative anesthetic, a dream-like state inducer, or a psychedelic medicine? One of our projects revisited a largely overlooked body of anesthesia literature to shed new light on how context influences ketamine’s effects. By tracing how different framings like “dissociative” and “psychedelic” emerged across clinical settings, we reveal how factors like language, dosage, and environment can profoundly shape both the subjective experience and the therapeutic outcomes of ketamine treatment.
- Diep, D., de la Salle, S., Thibault Lévesque, J., Lifshitz, M., Garel, N., & Greenway, K. T. (2025). The ketamine chameleon: history, pharmacology, and the contested value of experience. Expert review of clinical pharmacology, 18(3), 109–129. https://doi.org/10.1080/17512433.2025.2459377
Imprinting
Can the media we consume shape our psychedelic journeys? Yes! Through “imprinting”, recent environmental exposures, especially digital content, can influence the imagery and emotional tone of psychedelic experiences. Drawing on qualitative data from our clinical trial, we found that themes and visuals from media consumed in the days before treatment sometimes resurfaced during sessions, even altering therapeutic depth and direction. A broader literature review revealed that similar patterns have quietly appeared across decades of psychedelic research. By extending the classic “set and setting” model to include delayed contextual influences, we plan to further explore how our digital and behavioural habits before therapy may subtly shape outcomes.
- Garel, N., Thibault-Levesque, J., Sandra, D., Solomonova, E., Lifshitz, M., Richard-Devantoy, S., & Greenway, K. T. (2023). Imprinting: Expanding the extra-pharmacological model of psychedelic drug action to incorporate delayed influences of sets and settings. Frontiers in Human Neuroscience, 17, 1200393. https://doi.org/10.3389/fnhum.2023.1200393
Canadian & Global Psychedelic Survey
Music is a core component of psychedelic-assisted therapy, with clinical protocols recommending music use to be unfamiliar and lyric-free. The Canadian and Global Psychedelic Surveys are the first surveys to ask non-clinical populations about their psychedelic use. Our team developed music-specific questions to ask respondents about their music preferences and patterns of use when experiencing psychedelics, to gather information about the relationship between music and psychedelic use within a naturalist population. We’ve found that contrary to clinical protocols, respondents have little to no preference for unfamiliar and lyric-free music. Moreover, while music use is considered to be essential in psychedelic-assisted therapy, respondents have reported preferences for no music use or a combination of music and no music, depending on the type of psychedelic substance.
The MUSIK Trial
Music has been a nearly universal component of psychedelic therapies since their first development in the mid-20th century. Music is also often a core aspect of the Montreal Model of Ketamine-Therapy and was studied in our recent Randomized Clinical Trial: The Music for Subanesthetic Infusions of Ketamine (MUSIK) Trial.
This trial, conducted in Montreal between January 2021 and August 2022, compared carefully refined musical playlists to a matched form of non-music support centred on guided mindfulness and active dialogue. The MUSIK trial found that music was successful in reducing the blood pressure increases associated with ketamine, but both approaches were similarly effective overall, in terms of psychiatric benefits and sorts of psychedelic experiences.
However, the music and non-music approaches developed in the MUSIK trial may have highly person-specific effects, each offering unique advantages and disadvantages, further described on the Montreal Model Website.
- Greenway, K. T., Garel, N., Williams, L., Beaulieu, S., Turecki, G., Rej, S., & Richard-Devantoy, S. (2024). Music as an intervention to improve the hemodynamic response of ketamine in depression. JAMA Network Open, 7(2), e2354719. https://doi.org/10.1001/jamanetworkopen.2023.54719
ReSPCT Guidelines
Psychedelic science has long emphasized the importance of “set and setting”, that is, the patient’s mindset and the environment in which a psychedelic is taken, yet these factors are rarely reported in clinical trials. To address this gap, we developed the Reporting of Setting in Psychedelic Clinical Trials (ReSPCT) guidelines. Through a Delphi consensus process, 89 experts from 17 countries – including researchers, clinicians, and past trial participants – generated nearly 800 suggestions, distilled into 30 core variables. These span four domains: physical environment, dosing session procedures, therapeutic framework and protocol, and participants’ subjective experiences. The ReSPCT guidelines provide the first structured framework for documenting extra-pharmacological variables in psychedelic research. By improving consistency and transparency, they establish a benchmark for trial design and interpretation, strengthening both scientific validity and clinical relevance.
- Pronovost-Morgan, C., Greenway, K. T., Roseman, L., & The ReSPCT Experts. (2025). An international Delphi consensus for reporting of setting in psychedelic clinical trials. Nature Medicine, 31, 2186–2195. https://doi.org/10.1038/s41591-025-03685-9
Learn more
Social Determinants of Health
Social determinants of health, i.e., the conditions in which people are born, grow, live, work, and age, play a key role in shaping both an individual’s mindset and the environment in which psychedelic experiences occur. This impact is significant because psychedelic experiences are closely tied to an individual’s personal developmental trajectory and broader social-structural context. Calls to improve data collection and reporting have been hindered by practical constraints and lack of structured guidelines. Our group is addressing this challenge by developing a practical roadmap for integrating social factors into psychedelic neuroscience. We are combining expert consultation with a systematic review of current practices, which is currently underway. In October 2025, we held our first workshop to identify barriers and opportunities for better inclusion of social determinants in research and clinical practice, and to start building consensus around these guidelines. The expected outcomes include a tiered reporting system for social determinants in psychedelic research and a continuous learning model to strengthen collaboration between researchers and clinicians.
Learn more about the HBHL SDoH in Neuroscience Team Grant.
Establishing Standardized Measures for Psychedelic Medicine
As clinical care and research in psychedelic therapy expand rapidly, inconsistent data collection highlights the urgent need for standardized measures to build robust evidence and guide safe, equitable, and scalable practice. This project aims to create a standardized framework for collecting data in psychedelic therapy across clinical and research settings. In collaboration with the Psychedelics Mental Health Access Alliance (PMHA) and UC Berkeley’s Collaborative on the Economics of Psychedelics, we aim to address the critical need for consistent and comparable data in this field. By engaging a diverse international panel of experts, including clinicians, researchers, economists, and policy specialists, through a structured Delphi consensus process, the project will identify best practices for measuring outcomes, timing, and key variables in psychedelic therapy. The resulting framework, accompanied by an interactive online tool, will support more rigorous research, inform clinical guidelines, and guide policy and insurance decisions.
Interpersonal synchrony
The therapeutic relationship has long been recognized as a central ingredient of psychotherapy. To date, it has rarely been studied in depth in psychedelics-assisted psychotherapy. Our research therefore incorporates measuring this relationship as well as more subtle interpersonal dynamics that unfold within it: interpersonal synchrony, i.e. the spontaneous coordination of rhythms between two or more people, from language patterns to physiological signals such as heart rate variability. Using wearable sensors and computational analysis of dialogue, we aim to capture how patients and clinicians align such rhythms in real time during treatment sessions. These methods allow us to quantify aspects of the therapeutic encounter that are typically described only qualitatively, offering new precision in studying patient-clinician dynamics in psychedelic therapy.
Compassionate access study
Recent clinical trials show that psilocybin can alleviate anxiety and depression in people with life-threatening illnesses. Building on these findings, Canada created legal pathways for therapeutic access with psychological support. Our team conducted one of the first prospective studies of Canadians granted Section 56 exemptions for psilocybin-assisted psychotherapy. Eight participants with cancer diagnoses completed surveys before and after their sessions. Two weeks post-treatment, participants showed significant improvements in anxiety, depression, pain, quality of life, and spiritual well-being. While most described their experiences as highly meaningful, one reported reduced well-being. These early findings suggest that real-world psilocybin therapy outcomes mirror those seen in clinical trials, highlighting the need for continued evaluation as legal access expands.
- de la Salle, S., Kettner, H., Thibault Lévesque, J., Garel, N., Dames, S., Patchett-Marble, R., Rej, S., Gloeckler, S., Erritzoe, D., Carhart-Harris, R., & Greenway, K. T. (2024). Longitudinal experiences of Canadians receiving compassionate access to psilocybin-assisted psychotherapy. Scientific Reports, 14, 16524. https://doi.org/10.1038/s41598-024-66817-0
SAP program
Coming soon…
Tailoring & Patient Preferences (PPP)
Psilocybin-assisted psychotherapy (PAP) has emerged as a promising new approach for treatment-resistant depression. Early clinical trials suggest that PAP can produce rapid and durable antidepressant effects with a favourable safety profile. However, much remains unknown about how best to optimize the psychotherapy component of this intervention. Evidence from meta-analyses of psychiatric treatments indicates that adapting care to patients’ preferences can reduce drop-out rates, strengthen the therapeutic alliance, and improve outcomes, particularly given the role of sociocultural contexts in shaping treatment effectiveness and tolerability. In clinical practice, shared decision-making between patients and clinicians is a cornerstone of psychiatric care and is endorsed in medical guidelines, yet these considerations are often underrepresented in the design of clinical trials. Within PAP, nonpharmacological elements such as music and mindfulness are especially likely to be influenced by patient preferences. Tailoring these components in clinical trials to individual experiences and worldviews may enhance the efficacy, safety, and real-world applicability of PAP, helping to bridge the gap between controlled research settings and diverse clinical populations.
